Schizophrenia
Schizophrenia, a complex and enigmatic mental condition, challenges our understanding of the human psyche, inviting us to explore the depths of cognition and emotion. Its labyrinthine array of symptoms challenges our comprehension and leaves profound imprints on individuals, families, and communities. Schizophrenia stands as a testament to the complexity of the human brain, and just how far the boundaries of our reality can blur.
Schizophrenia represents a chronic and severe mental condition that profoundly impacts an individual’s cognition, emotions, and actions. Daily functioning is significantly compromised, disrupting multiple facets of life, such as work, relationships, and self-care.

An intricate interplay of multifaceted factors contributes to the aetiology of schizophrenia. Schizophrenia’s origins can be attributed to genetic predisposition and environmental influences. Although there isn’t a singular “schizophrenia gene,” a positive family history of the condition escalates the vulnerability. Furthermore, certain prenatal variables, such as maternal infections or inadequate nutrition, have also been identified as potential catalysts for susceptibility to schizophrenia.
Neurobiological factors have also emerged as significant contributors, with neurotransmitter imbalances, particularly dopamine and glutamate, being implicated. Brain imaging studies have revealed functional and structural abnormalities in various brain regions, further highlighting the intricate nature of the condition.
Schizophrenia symptoms often interfere with a person’s ability to think clearly, manage emotions, relate to others, and function effectively.
The symptoms of schizophrenia are typically classified into two main categories: positive signs and negative symptoms. It’s worth noting that the terms “positive” and “negative” in this context refer to the presence or absence of certain behaviours rather than their valence.
Positive Symptoms: Symptoms that represent an excess or distortion of normal functioning
- Hallucinations: Individuals with schizophrenia may experience hallucinations, which are perceptual experiences that occur without any external stimuli. Auditory hallucinations (hearing voices that others cannot hear) are common. Visual, olfactory, gustatory, and tactile hallucinations can also occur.
- Delusions: Delusions are false beliefs that are strongly held despite evidence to the contrary. These beliefs often involve themes of persecution, grandiosity, control, or bizarre thoughts. Delusions can significantly impact a person’s perception of reality and interactions with others.
- Disorganised thinking: Disorganised thinking is characterised by fragmented thought patterns, incoherent speech, and difficulty organising thoughts logically. This can make it challenging for individuals with schizophrenia to communicate effectively and express themselves coherently.
- Disorganised or abnormal motor behaviour: This category includes a range of behaviours such as unpredictable agitation, unusual postures, repetitive movements, and catatonia (a state of reduced responsiveness and lack of movement).
Negative Symptoms: Symptoms that involve a decrease or loss of normal functioning.
- Affective flattening: This refers to a reduction in the range and intensity of emotional expression. Individuals may appear emotionally distant, with limited facial expressions and vocal inflections.
- Alogia: Alogia involves reduced speech output. People experiencing this symptom may respond with brief or monosyllabic answers and exhibit impoverished speech content.
- Anhedonia: Anhedonia is the inability to experience pleasure or interest in previously enjoyed activities. Individuals may need more motivation to engage in hobbies or social interactions.
- Avolition: Avolition refers to a decrease in the initiation of purposeful activities. Individuals may struggle to start and complete tasks, leading to neglect of personal hygiene and responsibilities.
Cognitive Symptoms: Symptoms that affect a person’s thinking processes and can significantly impact their ability to plan, organise, and make decisions.
- Impaired concentration: People with schizophrenia often have difficulty focusing their attention and maintaining concentration on tasks.
- Impaired working memory: Working memory deficits can make it challenging to hold and manipulate information, affecting problem-solving and decision-making.
- Impaired executive functioning: This involves difficulties with planning, organising, and managing tasks. It can lead to disorganised behaviour and poor judgement.
Schizophrenia is a complex disorder whose symptoms can vary in intensity and manifestation, not all individuals with schizophrenia experience the same symptoms, and they can vary widely depending on the person.
Psychosis is a mental state characterised by a disconnection from reality, often involving hallucinations, delusions, and impaired thinking. While psychosis is not exclusive to any one disorder, it is a hallmark symptom of several mental health conditions, including schizophrenia.
Understanding the link between psychosis and schizophrenia is crucial for grasping the complexities of these conditions and their impact on individuals’ lives. This connection underscores the importance of early detection, proper diagnosis, and appropriate intervention to support those affected by these challenging mental health issues.
While not everyone experiences all of these stages, there are generally five stages that can describe the progression of psychosis:
- Prodromal: This is the earliest stage, marked by subtle changes in behaviour, thoughts, and emotions. Individuals in this stage might become increasingly withdrawn, experience social difficulties, and exhibit odd or irrational beliefs. This stage is often difficult to recognise as signs of impending psychosis.
- Acute: This is the stage when full-blown psychotic symptoms become apparent. Hallucinations and delusions are common during this stage. Thoughts may become disorganised, and emotional responses might be erratic. This stage often requires immediate medical attention, which can be distressing.
- Stabilisation: After the acute phase, some individuals experience a stabilisation of their symptoms, often with the help of medical treatment, therapy, and support. Medications and therapeutic interventions aim to reduce the intensity of hallucinations and delusions and address other related symptoms.
- Recovery: During this stage, individuals work on regaining their functioning and managing residual symptoms. Therapy, support groups, and lifestyle adjustments are crucial in promoting recovery.
Recovery stage: During this stage, individuals work on regaining their functioning and managing residual symptoms. Therapy, support groups, and lifestyle adjustments are crucial in promoting recovery.
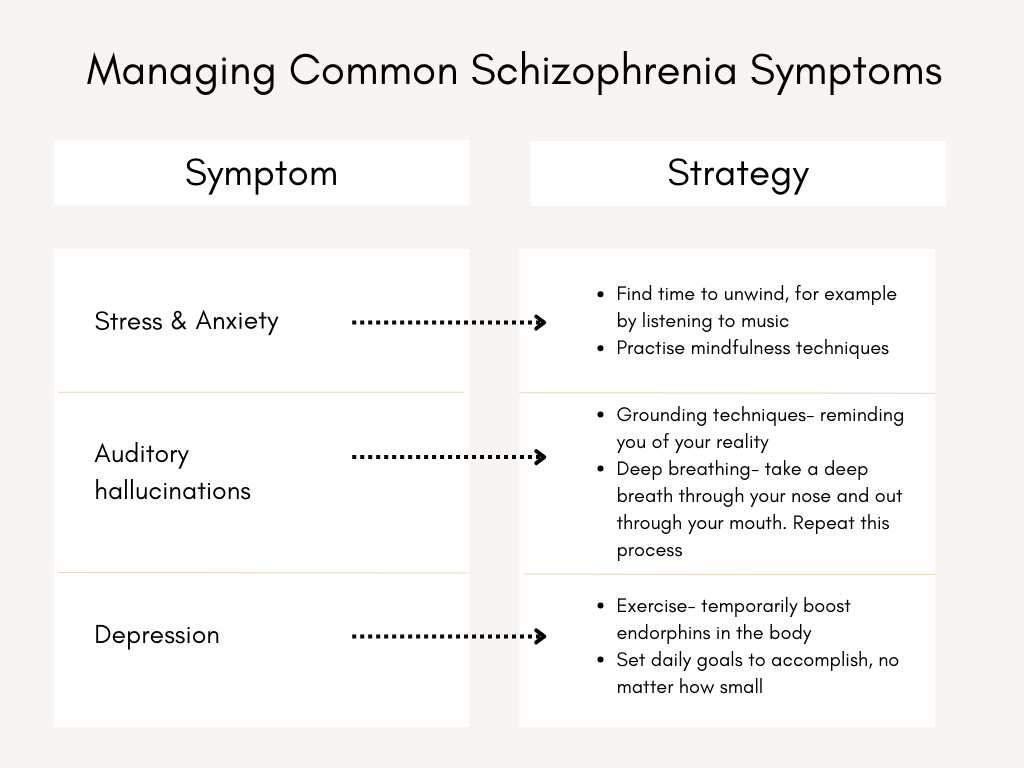
Schizophrenia is a complex mental health condition often demanding a comprehensive treatment strategy encompassing medication, therapy, and support. As such, seeking guidance from a qualified healthcare professional is imperative to receive personalised advice tailored to your needs. However, if you’re looking for strategies to alleviate specific symptoms of schizophrenia, you can consider the following approaches:
-
- Grounding techniques: Grounding techniques involve using sensory experiences, such as focusing on your breath, tactile sensations, or the present environment, to anchor yourself in reality and manage symptoms of schizophrenia, such as hallucinations.
- Deep breathing: A relaxation technique involving slow and controlled inhalation and exhalation can help alleviate anxiety and reduce the stress associated with schizophrenia symptoms, promoting a calmer and more balanced mental state.
- Distract yourself: Distracting yourself by listening to music, reading or participating in hobbies you enjoy can be beneficial as it shifts your focus away from distressing thoughts or symptoms of schizophrenia, allowing for temporary relief and a break from heightened emotional states.
- Positive self-talk: Self-talk involves consciously directing your internal dialogue and thoughts positively and constructively, which can help manage negative emotions and cognitive challenges often experienced with schizophrenia.
Seek support: Try to connect with a reliable individual who understands your circumstances, keeping you grounded while navigating the challenges of experiencing an episode.
Recognising the early warning signs of schizophrenia can help facilitate earlier intervention and better outcomes. It’s important to remember that experiencing one or more of these signs doesn’t necessarily mean someone has schizophrenia, but they can be indicative of the need for further evaluation by a mental health professional.
Some early warning signs of schizophrenia include:
- Social withdrawal: A noticeable decrease in social interaction, withdrawal from friends and family, and a loss of interest in previously enjoyed activities.
- Unusual beliefs or thoughts: Expressing odd or irrational beliefs that seem out of touch with reality, such as believing in conspiracy theories or supernatural experiences.
- Changes in speech patterns: Speaking incoherently or disjointedly, with unclear connections between thoughts, known as “thought disorder.”
- Heightened suspicion: Developing an excessive or unwarranted mistrust of others, often leading to feelings of persecution or paranoia.
- Perceptual disturbances: Experiencing sensory distortions, such as hearing voices that others don’t hear (auditory hallucinations) or seeing things that others don’t see (visual hallucinations).
- Emotional changes: Showing reduced emotions, such as flat affect (lack of emotional expression) or inappropriate emotional responses.
- Difficulty concentrating: Struggling to focus, concentrate, or follow a train of thought.
- Sleep patterns change: Experiencing disturbances in sleep, such as insomnia or an increased need for sleep.
- Irritability: Displaying heightened irritability, hostility, or anger without apparent cause.
- Lack of insight: An inability to recognise unusual or problematic thoughts or behaviours.
When you notice these signs, involving a mental health professional is crucial, especially if they persist or worsen over time. Early intervention and treatment can help manage symptoms and improve an individual’s quality of life. If you or someone you know is experiencing these symptoms, consider seeking guidance from a healthcare provider.
The diagnosis of schizophrenia involves a comprehensive assessment of an individual’s thoughts, emotions, behaviours and overall mental state. Conducted by trained mental health professionals, such as a psychiatrist or a clinical psychologist, the process follows diagnostic criteria outlined in classification systems such as the International Classification of Diseases (ICD). Clinicians gather information through interviews, observation, and sometimes collaboration with family members to understand the symptoms’ onset, duration and nature.
The diagnostic process involves ruling out other potential causes for the observed symptoms, such as substance abuse or medical conditions. Once a thorough evaluation is complete, a diagnosis can be made, and appropriate treatment strategies can be initiated to support individuals living with schizophrenia.
While only qualified mental health professionals can definitively diagnose or rule out schizophrenia, certain steps and considerations can help the process:
- Medical assessment: Certain medical conditions and substance abuse can mimic or exacerbate symptoms of schizophrenia. Medical issues like brain tumours, thyroid disorders, or drug interactions can lead to psychiatric symptoms. A medical assessment can help rule out these potential underlying causes.
- Duration and severity: Schizophrenia symptoms persist for a significant period, usually at least six months, and substantially impact a person’s functioning. A brief episode of symptoms triggered by a specific event might suggest a different diagnosis.
- Other psychiatric disorders: Some other psychiatric disorders, such as bipolar disorder, schizoaffective disorder, or certain personality disorders, can share symptoms with schizophrenia. A thorough evaluation helps differentiate between these conditions.
- Genetic factors: A family history of schizophrenia might increase the likelihood of developing the disorder, but it is not definitive.
- Substance use: Substance abuse, particularly long-term use of certain drugs, can induce psychotic symptoms. It’s crucial to consider the influence of substance use on the presentation of symptoms.
- Trauma and stress: Severe traumatic experiences or extreme stressors can lead to transient psychotic symptoms that might not indicate schizophrenia. Exploring the presence of such factors is essential.
- Developmental factors: In some cases, symptoms might be related to developmental or neurodevelopmental disorders rather than schizophrenia.
Remember, a proper diagnosis can only be made by qualified professionals through a comprehensive assessment. Getting an accurate diagnosis is crucial for appropriate treatment if you or someone you know is experiencing symptoms.
The goal of treatment for schizophrenia is not necessarily to “cure” the condition but rather to manage symptoms, improve quality of life, and enhance functional abilities. Many individuals living with schizophrenia can achieve significant improvements and maintain a level of functioning that allows them to lead meaningful lives.
UKAT London Clinic provides an array of therapeutic options tailored to assist individuals seeking effective management of schizophrenia.
Examples of the tailored therapeutic opportunities available at UKAT London Clinic are as follows:
- Cognitive Behavioural Therapy (CBT): CBT is a widely used psychotherapy approach to help individuals with schizophrenia manage their symptoms and improve their coping skills. It focuses on identifying and challenging negative thought patterns and developing healthier ways of thinking and behaving.
- Family therapy: Schizophrenia can have a significant impact on family dynamics. Family therapy can help improve communication, understanding, and support within the family unit, contributing to better outcomes for individuals with schizophrenia.
- Immersive therapy: Immersive therapy approaches, like equine therapy, offer individuals with schizophrenia a unique and experiential avenue for therapeutic growth. Engaging with animals or nature in a controlled and supportive environment can help enhance self-awareness, improve interpersonal skills, and foster emotional regulation. These immersive experiences can complement traditional therapeutic methods, providing individuals a holistic approach to managing their condition.
- Psychoeducation: Education about schizophrenia, its symptoms, and management strategies is crucial for individuals and their families. Psychoeducation programmes can enhance understanding and improve adherence to treatment plans.
- Holistic approaches: UKAT London Clinic can also offer holistic methods such as mindfulness, art therapy, and recreational activities to promote overall well-being and reduce stress.
At UKAT London Clinic, our distinctive approach involves meticulously tailoring treatment timetables and therapeutic interventions to align precisely with the unique requirements of each individual. Our team of experienced professionals employs a comprehensive assessment process to deeply understand each person’s needs, preferences, and challenges. Through this thorough evaluation, we identify the therapies that offer the highest potential for efficacy on their path to well-being.
Contact us today to learn more about how our bespoke treatments can support you.
